Flat Feet: Causes, Stages and Treatment
How To Tell if You Have Flat Feet
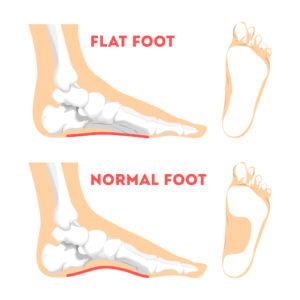
You have flat feet when the arch on the inside of your feet is flattened, allowing your entire foot to touch the floor when you stand up. A common and usually painless condition, flat feet may occur when the arches don’t develop during childhood. In other cases, flat feet may be caused by an injury or from the simple wear and tear stresses of age.
Flat feet can sometimes cause problems in your ankles and knees because the condition can force your ankles to turn inward and this throws off the alignment of your legs. If you aren’t experiencing any pain, no treatment is usually necessary for flat feet. However, symptoms can indicate tendon injury which will progress and cause osteoarthritis of the foot so the evaluation of flat feet is essential.
Meet Our Flat Feet Specialists
The foot and ankle specialists at Seaview Orthopaedics have helped many patients with flat feet and the issues that can arise from having flat feet. Schedule an examination with Dr. Aron Green, Dr. Eric Beights, Dr. George Fahoury, or Dr. Ian Hersh today!
Causes of Flat Feet
There are various causes for flat feet including:
- Genetics
- Weak arches
- Foot or ankle injury
- Arthritis or rheumatoid arthritis
- Damage, dysfunction, or rupture of the posterior tibial tendon
- Nervous system or muscle diseases, such as cerebral palsy, muscular dystrophy, or spina bifida
Flat feet can also develop as a result of medical conditions, such as pregnancy, obesity, or diabetes. Even age and the daily use of the feet can cause the posterior tibial tendon (the primary support structure for the foot arch) to weaken. If the tendon becomes inflamed (tendinitis) or tears after overuse, the damage to the tendon may cause the foot arch to flatten.
Symptoms of Flat Feet
Some patients who have flat feet never have symptoms, and never need treatment. Others may experience pain in the heel or arch area as a result of strained muscles and connecting ligaments. If the ankle turns inward, it may cause abnormal stresses on the knee and hip, resulting in pain in these joints as well.
Diagnosing Flat Feet
During your appointment, your doctor will ask you questions about your medical history and any medications you may be taking. As part of your physical examination, your doctor will examine the front and back of your feet and observe you as you stand and walk. Your doctor may also ask you to stand on the tips of your toes to examine the shape and function of each foot.
You may also be asked more specific questions about your condition, such as:
- Where does it hurt?
- How would you describe the pain – dull, sharp, burning?
- Does any specific motion or position make the pain worse?
- Do the shoes you wear affect the pain?
- Have you tried arch supports?
- How does the pain impact your life?
Imaging tests, such as x-rays, CT scans, ultrasound or an MRI may be ordered for you to determine the severity of your condition and/or whether or not you have arthritis or an injured tendon.
Signs and Stages of Flat Feet
The most common problem affecting patients with flat feet is posterior tibial tendinitis. This condition occurs when the posterior tibial tendon, which is responsible for maintaining arch height and toe raises, becomes inflamed.
Flat feet are categorized into four stages:
- Stage 1 – The posterior tibial tendon is inflamed, but the foot is not significantly flat.
- Stage 2 – The foot is flat, and the posterior tibial tendon is not functional. The arch can be recreated by actively correcting the foot, but there is a weakness in the tendon. Treatment is critical to prevent progression to Stage 3.
- Stage 3 – The patient has a rigid flat foot. The foot has lost flexibility because the joints are arthritic.
- Stage 4 – The foot is in either Stage 2 or Stage 3, but ankle arthritis is also present.
Treatments for Flat Feet
Our foot and ankle specialists recommend treatments based on the stage of flat feet. Treatments may range from noninvasive options to surgical intervention to help relieve foot pain and improve function for patients.
If you suspect you have flat feet, we recommend an examination and treatment as soon as possible. Treatment in the early stages of flat feet can prevent progression to the later stages.
Treatment of Stage 1 flat feet may initially include anti-inflammatories, rest, bracing, and physical therapy to try to alleviate the tendinitis. At Seaview, we offer physical therapy on-site at all of our practice locations for the convenience of our patients.
Additional nonsurgical treatments may include corticosteroid injections into the tendon sheath to alleviate symptoms and orthotics to help prevent tendinitis from recurring. At Seaview, we offer custom orthotics services as well.
If the tendinitis persists, surgical options such as a tenosynovectomy or a tenolysis of the posterior tibial tendon may be considered.
If the condition progresses to Stage 2, surgery is often recommended. Unfortunately, the longer posterior tibial tendinitis is present, surgery becomes more invasive and outcomes are less successful.
Patients with Stage 2 flat feet must receive treatment to prevent progression to Stage 3.
Surgery for a Stage 2 flat foot initially involves a tendon transfer. The flexor digitorum longus (FDL) tendon, the tendon that bends the tips of the little toes, functions similarly to the posterior tibial tendon and can be transferred to take the place of the posterior tibial tendon.
Once the tendon is repaired, your surgeon will need to correct the flattening of the foot to prevent the tendon from tearing. This is typically accomplished with a series of surgical procedures done in steps.
If the Achilles tendon is tight, your surgeon may recommend a procedure to lengthen it. The next step would be an osteotomy, which involves cutting the heel bone and shifting its position to recreate the arch in the foot. If the osteotomy does not completely recreate the arch, a lateral column lengthening may be recommended. This procedure is meant to lengthen the lateral column or outer portion of the foot. This can be done using bone grafts or metal implants.
If these procedures still do not adequately reconstruct the arch, subsequent procedures may include a cotton osteotomy to lengthen the medial column in the foot, or an arthroereisis to fine-tune the arch position.
If the patient’s condition progresses to Stage 3, a triple arthrodesis procedure may be considered. During this procedure, the three joints in the hindfoot are fused together to relieve pain. This eliminates motion in the hindfoot but preserves motion in the ankle and midfoot.
Patients with a Stage 4 flat foot will need treatment to address the ankle arthritis in addition to correcting the flat foot, as outlined above. Ankle arthritis can be treated either with ankle fusion or ankle replacement, depending on the extent of arthritis.
Flat Feet Treatment in Central New Jersey and Jersey Shore
Our board-certified foot and ankle team at Seaview Orthopaedics offers a full range of nonsurgical and surgical treatments for flat feet. Dr. Aron Green, Dr. Eric Beights, Dr. George Fahoury, and Dr. Ian Hersh are happy to help with all of your treatment needs. If you would like to Book Appointment with Dr. Green, Dr. Beights, Dr. Fahoury, or Dr. Hersh at one of our six New Jersey office locations, you cant contact us online, call us at (732) 660-6200, or visit one of our orthopedic clinics in person. Whichever you choose, we look forward to helping you!
Schedule An Appointment with Our Flat Feet Specialists





