Orthobiologics Used to Treat Musculoskeletal Injuries
What is Orthobiologics?
Orthobiologics are cells, substances, and materials that orthopedic surgeons use to help injuries heal more quickly. When used in higher concentrations they may help speed up the healing process of broken bones, injured muscles, tendons, and ligaments (musculoskeletal injuries). These products, made from substances that are naturally found in your body, also help to improve the quality of healing, offering better and stronger tissue and less scar tissue.
What is involved in the healing process?
When you have a musculoskeletal injury, there is bleeding in the injured area. This bleeding is the foundation for the healing response, and it provides a way for healing factors to reach the injury site. These healing factors (orthobiologics) in combination with bleeding are all necessary for healing. They include Matrix Materials, Growth Factors, and Stem Cells.
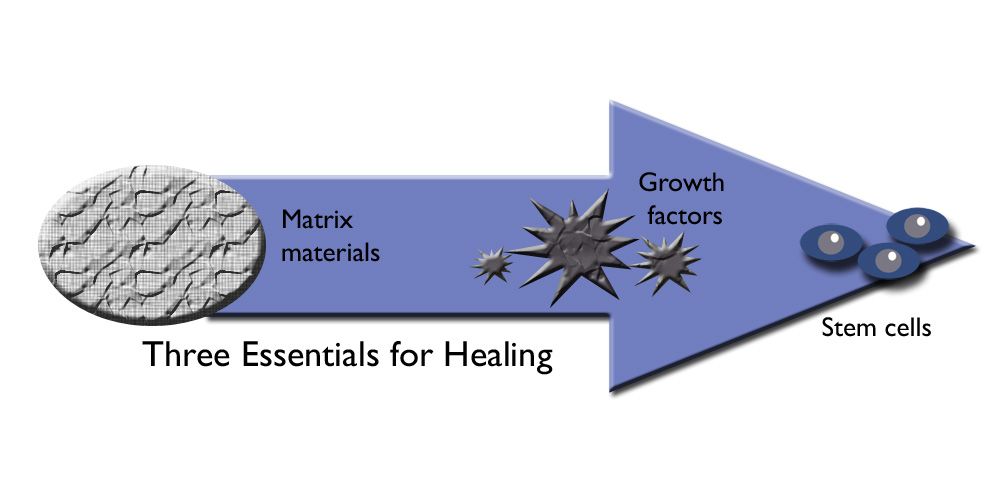
What is matrix material?
Matrix material (or conductive material) provides housing for stem cells while they grow into mature cells. If stem cells do not have a house to grow in, they cannot develop into repair cells that can heal bone, muscle, tendon, or cartilage.
When a patient breaks a bone, the healing process begins, and stem cells should be able to make new bone and promote healing. However, if a significant portion of the broken bone is lost due to a bone being crumbled or broken into several pieces protruding through the skin, a large gap may result. In this instant, the gap must be filled with matrix to house stem cells. There are several substances that can be used to fill such gaps, including:
Bone Grafts. There are two types of bone grafts–an autograft and an allograft.
An autograft is a bone graft that is harvested from the patient, usually taken from the patient’s iliac crest, which is a part of the pelvis. Harvesting the bone graft requires an additional incision during the operation to treat the injury. This not only increases the time of surgery but it can also cause increased pain or risk of infection after the operation. Generally, patients have a good outcome; however, the harvesting site usually takes a while to heal.
An allograft is a bone graft that comes from cadaver bone supplied by a bone bank (bone tissue that is donated upon death). If the needed bone graft is available, this is the preferred method, as it avoids the risk of pain at the donor site.
Artificial Matrix Material. Artificial matrix material, such as calcium phosphate, can also be used to fill a large void between bone ends. It can form a material that closely resembles bone, and it contains holes that are the right size for stem cells to enter and develop into mature cells.
What are the growth factors?
Growth factors are proteins. They play an important role in the healing process, as they call stem cells to the injury site to develop repair cells. This process is called chemoattraction.
Chemoattraction only works well when there is sufficient blood supply around the injured area for the protein to attract the stem cells, providing a way to travel to the area where they are needed.
When there is insufficient blood supply, we rely on regenerative medicine to explore ways to help the body heal better–harnessing the power of the body to heal and then accelerate it in a clinically relevant way.
Bone Morphogenetic Proteins (BMPs). BMPs are genetically engineered proteins that aid in bone healing. These synthetic proteins help with muscle, tendon, and cartilage healing. In large enough quantities, they are effective in speeding up the healing process of damaged bone, especially in fractures that have a difficult time healing.
What are stem cells?
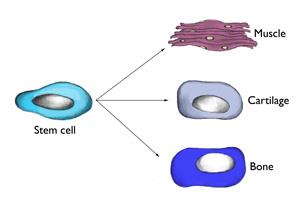
Stem cells are undifferentiated cells that are capable of giving rise to indefinitely more cells of any type. These immature cells can develop into many different cell types in the body and have the greatest potential for promoting healing, as they function as an internal repair system replenishing other cells where needed to promote healing. Each divided cell, therefore, has the potential to become another type of cell needed to help in healing–bone, muscle, ligament, and cartilage.
How can stem cells speed up the healing process?
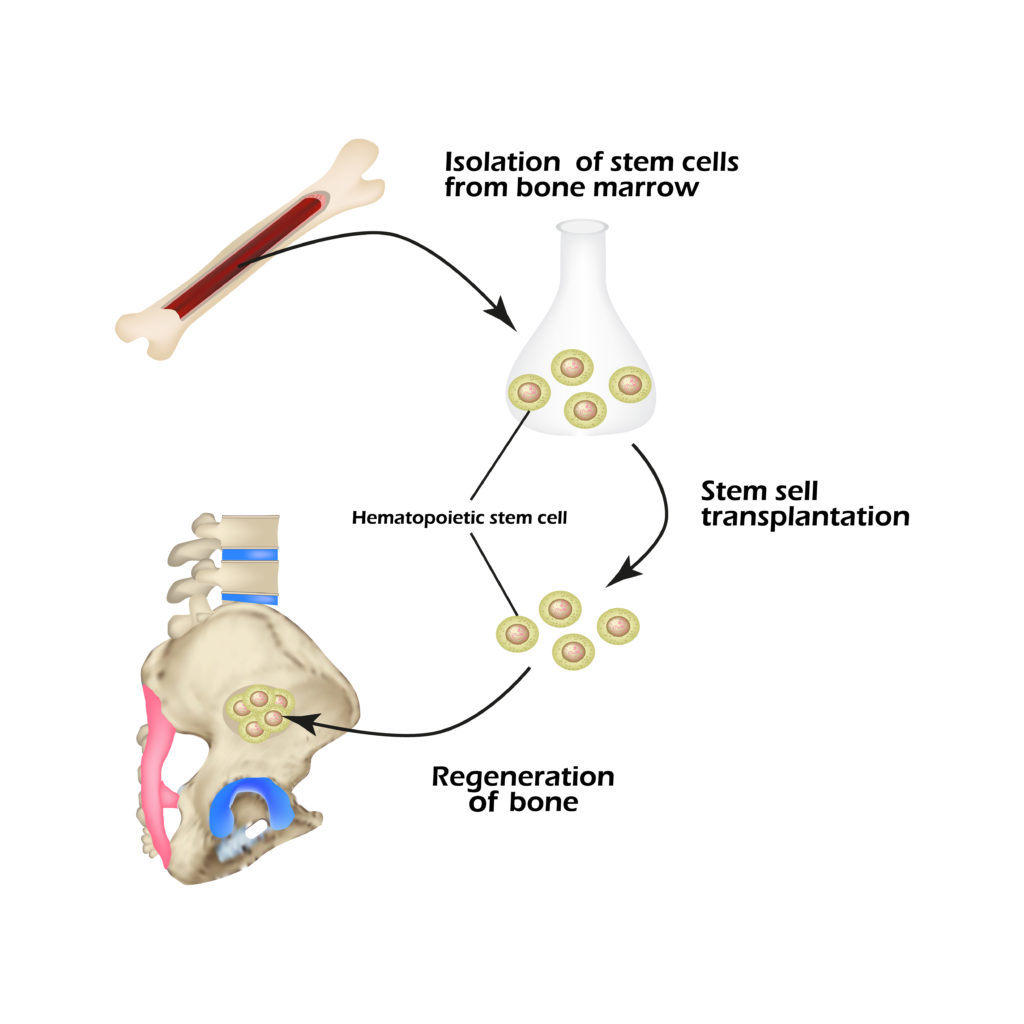
Doctors have developed ways to retrieve stem cells and deliver them to the injury site faster and in greater numbers and concentration to speed up the healing process. Stem cells can be retrieved either from harvesting them from a patient or through a stem cell donor program.
Stem Cell Harvesting. Stem cells can be harvested from bone marrow located in the centers of long bones, such as the bones in your arms, forearms, thighs, and legs. They can also be harvested from the pelvic bone, which contains the highest concentration of stem cells.
Once stem cells are drawn out of the bone marrow with a needle, the orthopedic surgeon inserts this large supply of stem cells into the injury site.
Stem Cell Donation. Doctors can also use donated stem cells to promote healing. These donated cells come from donors after they pass away. When the cells are harvested, they are treated so that they will not create an immune or allergic reaction in the patient.
How do we justify the use of stem cells?
Evidence-based medicine justifies the use of stem cells. We rely on evidence in making clinical decisions and integrating this evidence with clinical experience.
What is evidence-based medicine?
Evidence-based medicine is the conscientious, explicit and judicious use of the current best evidence in making decisions about the care of individual patients. The practice of evidence-based medicine means integrating individual clinical expertise with the best available external clinical evidence from systemic research.
How do you determine the best evidence?
The most controversial aspect of evidence-based practice is that individual studies frequently contradict each other. It is, therefore, our jobs as clinicians to determine which studies provide the best answer, evaluating study design and absence of bias.
The general principles for determining the best studies and evidence are those that are controlled versus uncontrolled, prospective versus retrospective, and randomized versus non-randomized.
Which stem cells do you use?
There are two stem cell categories, embryonic and mesenchymal.
Embryonic Stem Cells are harvested from human embryos grown in vitro (refers to the technique of performing a given procedure in a controlled environment outside of a living organism). They are pluripotent, meaning they have the ability to become a cell for any part of the body (nerve, muscle, blood, etc.). These stem cells are not used for treatment in the United States.
Mesenchymal Stem Cells (MSCs) are adult stem cells. They are multipotent (not pluripotent), meaning they have the ability to develop specific types of cells, for example, a blood stem cell can develop into a red blood cell. MSCs can differentiate in vitro into tendon and ligament cells, muscle cells, bone cells, cartilage cells, and fat cells.
How are mesenchymal stem cells retrieved?
MSCs are retrieved from Bone Marrow Aspirate Concentrate (BMAC) aspirated from the iliac crest, and adipose (fat) tissue derived from the abdomen or infrapatellar (below the patella–the bone at the front of the knee) fat pad.
A Lipogems System may be used to harvest MSCs from adipose tissue.
Are there any misconceptions about mesenchymal stem cells?
One of the biggest misconceptions about MSCs is that the stem cells directly convert into the diseased or injured tissue in question, and the
- Injection of MSCs in an osteoarthritic knee contributes directly to the regeneration of cartilage tissue; and
- Infusion into cardiac patients of MSCs will directly convert into functional heart muscle cells to replace the cells that die from the ischemia of the heart attack.
To clarify, MSCs after injection
- Do hone in on active sites of injury or inflammation.
- Do not differentiate into the tissue at that site.
- Do secrete bioactive factors.
- Do stimulate local stem cells to make healing tissue.
- Do offer therapeutic effects that can be analyzed as site-specific clinical outcomes.
What is the future for orthobiologics for musculoskeletal injuries?
Orthobiologics are a fertile field for stem cells and are effective in treating
- Focal chondral defects
- Early osteoarthritis
- Fractures
- Soft tissue injuries including tendons (e.g., rotator cuff tears), muscle and ligaments
In fact, the results of the case series studies published in the Journal of Arthroscopic and Related Surgery in 2013, were encouraging and showed that intra-articular injection of infrapatellar fat pad–derived MSCs is effective for reducing pain and improving knee function in patients being treated for knee osteoarthritis.
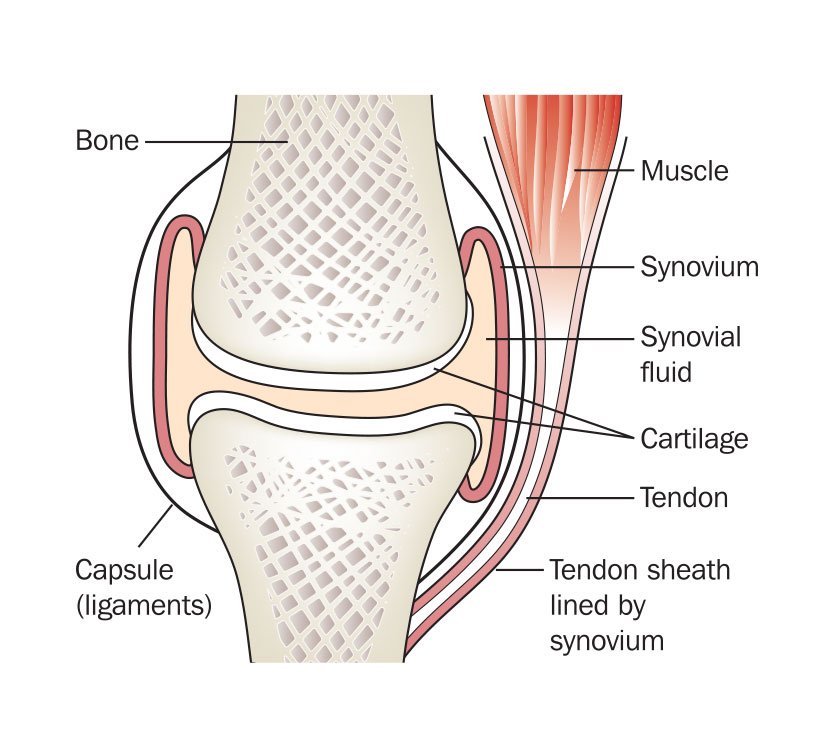
What are the pain generators for osteoarthritis?
There are three major pain generators for osteoarthritis
- Synovitis (see synovial joint diagram below)
- Subchondral bone lesions
- Loss of cartilage thickness (e.g., bone on bone)
What is the impetus for the use of mesenchymal stem cells in rotator cuff surgery?
The impetus for the use of MSCs in rotator cuff surgery is due to
- A high re-tear rate after repair of rotator cuff tears (40-60%) at 1-year post-op.
- Most rotator cuff tears are degenerative.
Under what circumstances would rotator cuff surgery with the use of MSCs be more beneficial?
Rotator cuff surgery with the use of MSCs would be most indicated for revision rotator cuff repair cases, for older patients, and for patients who are diabetics or smokers.
How effective is rotator cuff surgery with the use of MSCs?
In a case-controlled study as published in International Orthopedics in 2014, researchers found that patients who received concentrated bone marrow-derived MSCs as an adjunct to rotator cuff repair (RCR) at the time of arthroscopy better healed (87%) than patients who had RCR alone (44%). These patients also had a lower incidence of re-tears at 10-year follow-up.
What can Seaview Orthopaedics do for you?
Seaview Sports Medicine, a specialized medical practice of Seaview Orthopaedics, uses orthobiologics to treat musculoskeletal injuries. If you are interested in these regenerative medicine approaches to healing, give us a call today at (732) 660-6200 to schedule a consultation with one of our orthopedic sports medicine surgeons.
How effective is rotator cuff repair combined with Platelet-Rich Plasma (PRP)?
In a recent study published in the American Journal of Sports Medicine, researchers found that current evidence indicates that the use of PRP in rotator cuff repair results in improved healing rates, pain levels, and functional outcomes.
Contact Our Orthopedic Orthobiologics Specialists
If you are interested in Regenerative Medicine, please call Seaview Orthopaedics at (732) 660-6200 to schedule a consultation with Dr. Chern or one of our other Seaview Sports Medicine specialists.

